CNBC
As a phlebotomist at Northwell Health, a New York-based non-profit healthcare provider, my job is to draw blood from people, ensuring that the right amount is taken and that everything is properly labeled.
Like everyone else in this field, I’m comfortable around blood, needles and test tubes. But recently, I had to be OK with something entirely new: Testing patients for COVID-19.
“How do you feel about the coronavirus? Does it scare you?” my supervisor asked me earlier this month.
“Yes,” I said. “Of course it scares me.”
He told me that Northwell Health needed volunteers to trade in their usual duties to work at New York’s first drive-thru COVID-19 testing center. The site, which opened on March 13, is located in the middle of Glen Island Park in New Rochelle, an epicenter of the outbreak when the coronavirus first emerged in the state a few weeks ago.
After giving it some thought, I decided to do it. My husband wasn’t happy about it. I have three children and two stepchildren, including a 10-year-old son.
The job comes with a lot of risks, and the last thing I’d want is to get infected and potentially spread it to my family. But this pandemic is much bigger than me; it’s a situation that requires all hands on deck.
A typical day at the COVID-19 drive-thru testing site
For the past week and a half, I’ve been working 12-hour shifts — swabbing patients for COVID-19. My commute to the testing site is about a 30-minute drive from where I live in Queens over the Long Island Sound.
Things have been changing rapidly in terms of how the tests are administered. But the drive-thru approach is a way to test people so they don’t walk into an emergency room and infect other people.
Right now, there are six lanes available for cars to line up at the testing site. Keeping a safe distance from the cars, state troopers call out over megaphones to signal to drivers when it’s their turn. All visitors must stay in their vehicles with the windows closed.
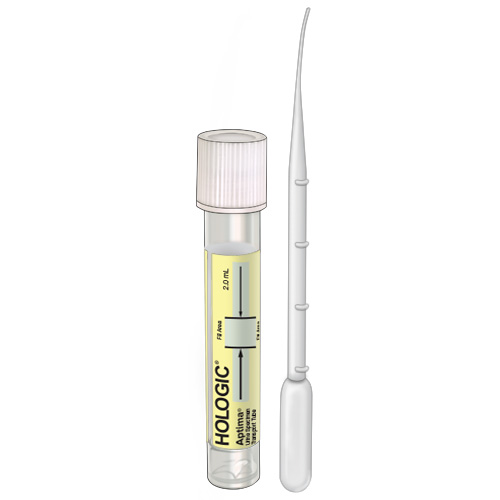
Once a car pulls up to the testing zone, they’re asked to roll down the windows. Each person, while still remaining in their seats, tips their head back as I conduct a series of nasal swabs. (Prior to the pandemic, only nurses and doctors were allowed to do the swabbing, so I had to train for the procedure. It’s a delicate process, and just one mistake could lead to test result errors.)
The other day, a family drove up with five kids in the car. The youngest, probably around seven years old, started to tear up. We tested the parents first so they could put on a brave face. Then we did the older daughter, who looked about 14. When we got to the fourth daughter, she started bawling hysterically.
“Would you like to sit with her?” I asked her mom.
“I don’t want to do this,” the daughter said. You could just see the look of fear on everyone’s faces. But then the mother hugged her daughter and said, “What’s scarier than not knowing? After this gets done, you’re done. The fear will be over.”
Scenes like that really tug at your heart.
Every three hours, couriers from BioReference Laboratories pick up the samples and transport them in cooler boxes to Elmwood Park, New Jersey. At the lab, the specimens are recorded and tested. Patients typically receive results in two to three days.
In order to get tested, residents must make an appointment by calling the New York State Coronavirus Hotline. On average, we’re collecting more than 1,000 samples per day. Other health systems and organizations are cycling through to help with demand as well.
Precautions we’re taking
I consider myself lucky: Northwell Health is doing a really good job at keeping everyone as safe as possible. I wear gloves and a jumpsuit that protects my entire body, along with a Powered Air-Purifying Respirator — a special face shield equipped with a respirator that cleans contaminated air before circulating it inside the suit.
(It’s the same type of protective gear used during Ebola-testing, and it’s a lot more comfortable than other air-shield masks — which makes a huge difference, especially when you have to wear it while standing all day.)
When I get home, I sanitize everything and take a shower. I do whatever I can to make sure there’s no risk of anyone getting contaminated. Each time someone enters the house, I tell them to wash their hands and then clean the door handles with disinfectant spray.
‘A lot of fear, yes, but mostly gratitude’
My two-week rotation will be up soon. After that, we reevaluate and discuss whether I continue at the testing site or return to my regular phlebotomist duties. If I’m asked to keep volunteering, I’ll say yes in a heartbeat.
When my 32-year-old daughter said I was crazy for doing this, I told her, “Imagine if you were sick right now, and the doctor ordered you to stay home until it passes. You don’t know whether it’s COVID-19 or the regular flu. Wouldn’t you prefer to have someone to test you right away, instead of waiting around with so much uncertainty?”
“Yeah,” she sighed. “I’d want to get tested.”
“Well, in order for that to happen, you need people who are willing test you,” I said. “And that’s what I’m doing for everyone else. It’s my job to help people.”
Every day, I see all kinds of expressions on people’s faces. There’s a lot of fear, yes, but mostly gratitude. They all leave and say, “Thank you. Thank you so much for what you’re doing.”
Vivian Velasquez-Caldera is a phlebotomist at Northwell Health. She lives in Queens, New York.
—Caroline Hopkins contributed to this story. Caroline is a health writer based in Brooklyn, New York. She has written for HealthDay, the American Society of Clinical Oncology, Daily News, SurvivorNet and Women’s Health Magazine.
Click here for original post on CNBC